
![]()
 NaviNet® is always your first stop for eligibility and benefit information, to check your allowances for the services you’re providing, to request needed authorizations, to submit and check the status of claims, and much more.
NaviNet® is always your first stop for eligibility and benefit information, to check your allowances for the services you’re providing, to request needed authorizations, to submit and check the status of claims, and much more.
But can you name the additional capabilities that NaviNet offers? In this issue of Provider News, as well as upcoming issues, we’re going to respond to your questions by focusing on some of the underutilized tools that are embedded in NaviNet. In this issue, we’ll show you how you can access a Highmark member’s health reimbursement account (HRA) information. We’ve also included a reminder of the retrospective (retro) review process for imaging services.
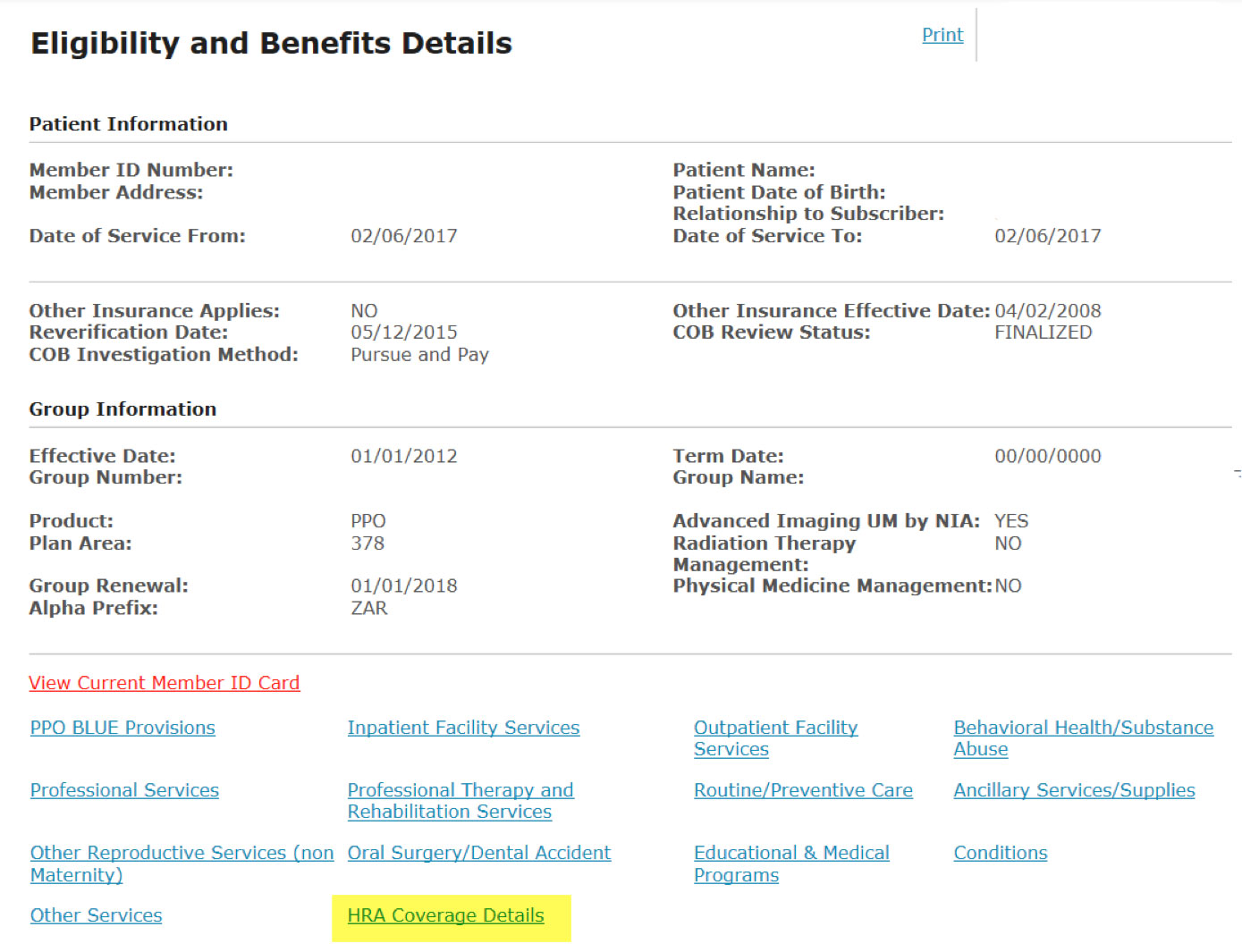
Many Highmark members now have plans with high deductibles that are tied to corresponding HRAs. You can easily tell if a member has an available HRA and access that information using NaviNet. To retrieve a member’s HRA information, select HRA Coverage Details (highlighted in yellow in the screen capture below) from the Eligibility and Benefits Details page.
The HRA Coverage Details page shows the amounts for both the Individual and Family Annual Election. If the HRA is partially funded by the member’s employer, this page will show any amount that the member (employee) is required to pay. Please note that you will have to contact Highmark to determine if the member has met any of the HRA amounts listed.
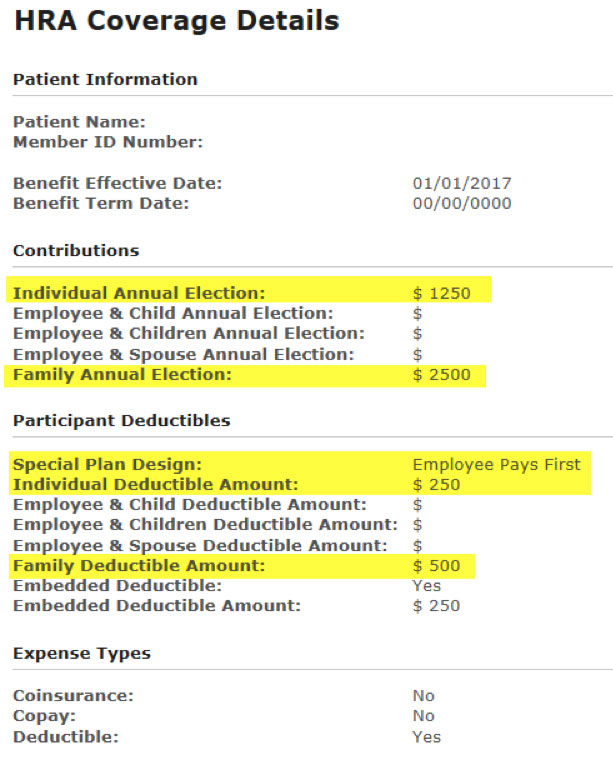
If a member’s HRA has been set up as “Direct Pay to Provider,” payment will be made directly from the HRA to the provider.
Providers can request that National Imaging Associates Inc. (NIA) perform a retro review of a member’s imaging scan for one of two reasons:
1. The ordering provider did not contact NIA prior to the service being performed, but calls NIA after the services have been performed.
2. The performing provider is requesting a retro review because a claim denied based on no authorization being on file.
Providers who are not yet NaviNet-enabled must call Highmark Customer Service at 1-800-346-6262, Option 6, after the approved authorization is provided by NIA and request that an adjustment be made.
Complete information about the Radiology Management Program and the retrospective review process can be found in the Highmark Radiology Management Program section of the Provider Resource Center.
For more complex issues, the Provider Service telephone lines offer expanded functionality to better serve you. Innovative self-service prompts allow you to get the detailed information that you need quickly and efficiently.
If you don’t have NaviNet, we strongly encourage you to visit navinet.net  and gain access to the system. Current NaviNet users who have questions about the system may call 1-888-482-8057 to speak with a NaviNet representative.
and gain access to the system. Current NaviNet users who have questions about the system may call 1-888-482-8057 to speak with a NaviNet representative.