
Many Highmark members now have health plans with high deductibles that are tied to corresponding health reimbursement arrangements (HRAs). You can easily tell if a member has an available HRA and access that information using NaviNet®.
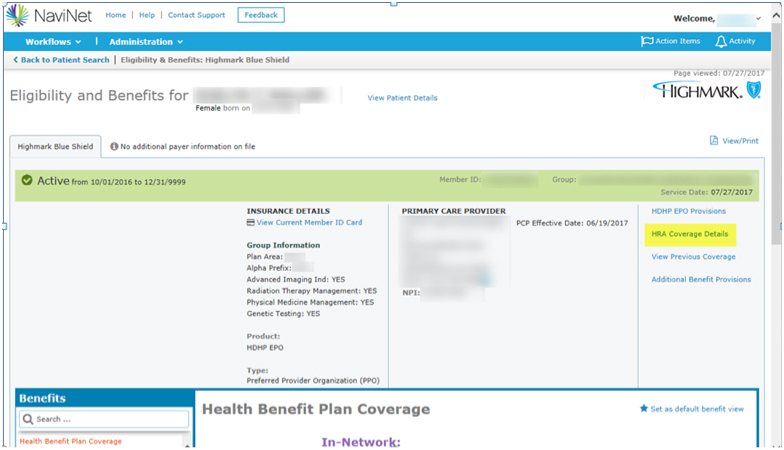
To retrieve a member’s HRA information, select HRA Coverage Details (highlighted in yellow in the screen capture below) from the Eligibility and Benefits Details page.
The HRA Coverage Details page shows the amounts for both the Individual and Family Annual Election. If the HRA is partially funded by the member’s employer, this page will show any amount that the member (employee) is required to pay. Please note that you will have to contact Highmark to determine if the member has met any of the HRA amounts listed.
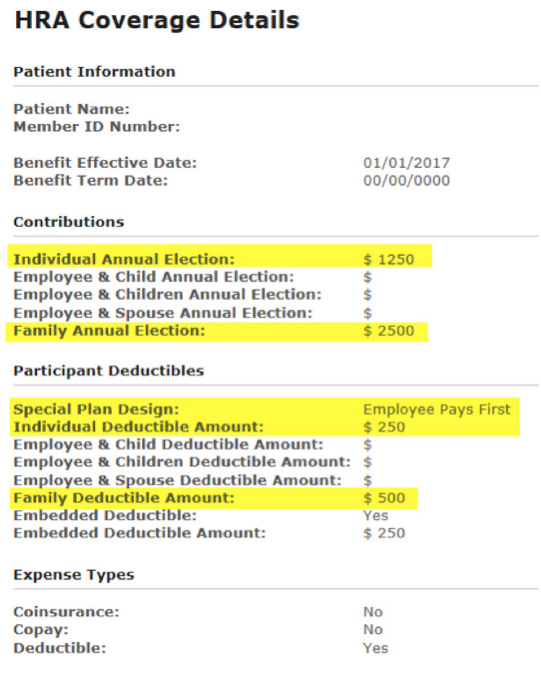
If a member’s HRA has been set up as “Direct Pay to Provider,” payment will be made directly from the HRA to the provider if the HRA has an account balance.
If you don’t have NaviNet, we strongly encourage you to visit navinet.net  and gain access to the system. Current NaviNet users who have questions about the system may call 1-888-482-8057 to speak with a NaviNet representative.
and gain access to the system. Current NaviNet users who have questions about the system may call 1-888-482-8057 to speak with a NaviNet representative.
In addition to using NaviNet to look up members’ HRA information, you can use the system to quickly locate eligibility and benefit information, to check your allowances for the services you’re providing, to request needed authorizations, to submit and check the status of claims, and much more.